The Doris Duke Charitable Foundation (DDCF) is pleased to announce the completion of the first major milestone of the African Health Initiative (AHI) data sharing plan: the public release of baseline data from all five of the AHI’s Population Health Implementation and Training (PHIT) health system strengthening projects. We encourage those interested in viewing the data to do so by visiting the Harvard Dataverse network here: African Health Initiative Dataverse. This data will complement the endline data that will be shared in 2017.
The AHI has released this data in direct support of calls for a data sharing revolution within the global public health sector by a number of funders of health research, major health journals and international institutions. With the conviction that data sharing of this kind holds the potential to advance progress in public health efforts, the AHI ascribes to the Joint Statement of Purpose laid out by the World Health Organization (WHO) in partnership with the Wellcome Trust. This common set of goals and principles for research funders aims to make “…data sets available to investigators beyond the original research team in a timely and responsible manner” and “…promote the efficient use of those data to accelerate improvements in public health.” Leading institutions, including the Council on Health Research for Development and the INDEPTH Network, have long made the case for the importance of sharing public health data and have requested support from funders to support such efforts.
The following update details the evolution of the AHI data sharing plan, an overview of the indicators that are being collected across projects and our plans for sharing the AHI’s endline data, which will show the extent to which the interventions have an impact on population health. We hope that many of our funding colleagues will find this information relevant as they consider their own systems for creating and increasing public access to the health research they support and that those public health funders not currently making data accessibility a priority will be inspired and encouraged to do so.
AHI data sharing plan
 In 2009, DDCF awarded each of the five PHIT Partnerships working to strengthen health systems in Ghana, Mozambique, Rwanda, Tanzania and Zambia with a grant of $8 million to $12 million. The PHIT interventions build on existing partnerships and opportunities within each country and therefore vary in design, but they share similar areas of focus and all aim to improve integrated primary care delivery, significantly reduce mortality and morbidity, and strengthen health systems across all levels in implementation districts. Each of the projects has evolved over the course of implementation, responding to their changing contexts. All project teams are conducting rigorous impact evaluations to contribute to the global learning agenda and to ensure that the results further the advancement of health services in systematic and sustainable ways. More details on the country-specific approaches being implemented and evaluated are available in the BMC Health Services Research Journal Supplement published in 2013.
In 2009, DDCF awarded each of the five PHIT Partnerships working to strengthen health systems in Ghana, Mozambique, Rwanda, Tanzania and Zambia with a grant of $8 million to $12 million. The PHIT interventions build on existing partnerships and opportunities within each country and therefore vary in design, but they share similar areas of focus and all aim to improve integrated primary care delivery, significantly reduce mortality and morbidity, and strengthen health systems across all levels in implementation districts. Each of the projects has evolved over the course of implementation, responding to their changing contexts. All project teams are conducting rigorous impact evaluations to contribute to the global learning agenda and to ensure that the results further the advancement of health services in systematic and sustainable ways. More details on the country-specific approaches being implemented and evaluated are available in the BMC Health Services Research Journal Supplement published in 2013.
An essential component of the AHI was the development of a “Data Collaborative” to promote cross-site learning. The Data Collaborative membership, as shown in Figure 1, includes the country- and US-based co-principal investigators, the DDCF program staff and a central and independent coordinating unit led by Drs. Jennifer Bryce, Bob Black and Larry Moulton from the Institute for International Programs at the Johns Hopkins University. The coordinating unit, referred to as the “Data Coordinator,” was created to serve as an external layer of data review for the AHI and an additional resource that the PHIT teams can draw on for design challenges and statistical questions. Responsibilities of the Data Coordinator include the identification of common measures, called “core metrics,” the development and maintenance of the Data Collaborative database, the promotion of cross-site learning and the facilitation of data sharing via the agreed-upon protocol.
The Data Collaborative’s Processes and Guidelines for Shared Data reflect DDCF’s greater commitment to sharing public health data. The guidelines provide specifications for a data management plan; a process for the timely submission of data, ethics and confidentiality standards; use of public databases and a central repository; and expectations for compliance to the data sharing policy, which requires partnerships to formally agree to submit data along with relevant documentation to a central database.
Baseline core metric data
The baseline database now available on the Harvard Dataverse website comprises 24 core metrics as defined in the Data Collaborative concept paper. The core metrics, which were adopted by the Data Collaborative in February 2011, are quantifiable health system indicators measured by all five PHIT Partnerships. The core metrics are organized according to the health systems strengthening model pictured in Figure 2. The conceptual model outlines the generalizable components under which the effectiveness of the PHIT team strategies is evaluated, namely via inputs and processes, outputs, outcomes and impact.
The “impact” component is particularly important as it holds the projects to a uniform standard of demonstrating a population health impact. The core metrics for health impact as defined by the collaborative are: (1) the under-five mortality rate, including the cause of death distribution in children under five; (2) child defined as the prevalence of stunting (low height for age) and wasting (low weight for height); and (3) the total fertility rate.
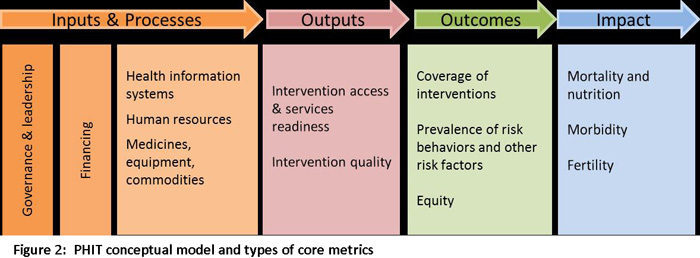
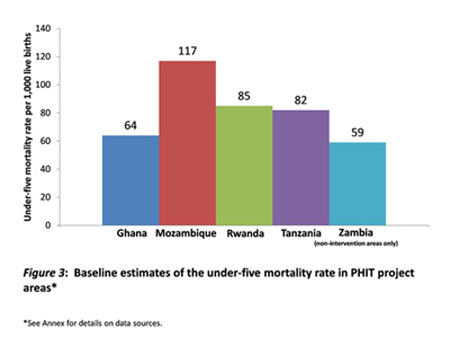
Figure 3 specifically addresses the under-five mortality data, showing that there was considerable variation across the PHIT intervention areas. Under-five mortality ranged from 118 per 1,000 live births in Mozambique to rates below 65 per 1,000 live births in Ghana and Zambia.
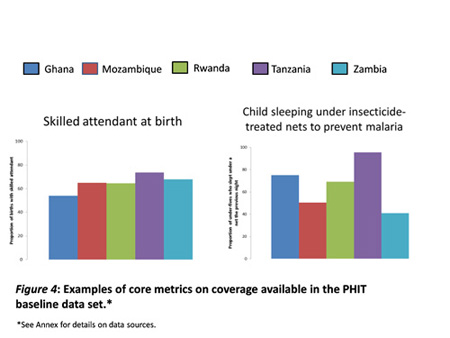
The PHIT projects are also collecting important core indicators that measure health outputs and outcomes. Figure 4 presents two examples of core metrics that examine other outcomes, showing the proportion of the population in PHIT intervention areas that received specific services. The graph on the left shows that, in all settings, only about six in 10 women had a skilled attendant present during delivery. The graph on the right shows that despite the fact that malaria is highly endemic in all sites, in some—like Tanzania—a high proportion of children under age 5 were reported to be sleeping under an insecticide treated net to prevent malaria, whereas in Rwanda and Zambia fewer than 50% of children are protected in this way.
Details on the data sources and time periods for the before-mentioned indicators are available in the Annex. Comparing these and other baseline indicator levels with those measured at the end of the project will support careful analysis of the contributions of each set of interventions to improvements in population health.
Next steps
Over the last two years, the PHIT teams have published peer-reviewed articles using baseline data in high-impact health journals, and they will continue to do so. A list of publications from the PHIT Partnerships can be found here: African Health Initiative Resources. In addition, they are working to address important implementation research questions that can only be answered using data from multiple sites. These cross-site analyses may address whole strategies or component parts of PHIT projects, and will inform multiple levels of learning (e.g., policy, organizational, process and population impact) about enhancing health and reducing mortality.
The AHI is committed to promoting the use of PHIT data to improve public health programs in low and middle income countries. National institutions based in the countries where the PHIT projects operate—specifically schools of public health, ministries of health and national offices of statistics—will be the most important users of this expanding data set.
Each of the PHIT projects will conduct a final round of data collection by 2016. Endline data will be released using a process and timeframe similar to those used for the baseline data. Consequently, open access baseline and endline datasets will allow for direct analysis of the PHIT Partnership health system strengthening initiatives and their impact on population health. With this timeframe in place, the DDCF will maintain its commitment to assuring that the larger public health community has timely access to these data so that further analyses can advance understanding of ways to strengthen health systems for the delivery of comprehensive primary care. It is our hope that DDCF will serve as a catalyst to increase funder support for genuine data sharing to improve population health.